Abstract
Background: Over the last five decades, pediatric acute leukemia survival rate improved significantly. However, serious long-term complications may occur in some patients and long-term follow-up strategies were implemented. Subgroups of patients with relapse, central nervous system (CNS) irradiation or hematopoietic stem cells transplantation (HSCT) are at high-risk of long-term complications and probably require lifetime follow-up. In contrast, the optimal follow-up of the large subgroup at lower risk of long-term complications remains poorly defined. Prolonged follow-up in this subgroup may lead to unnecessary medical visits, increasing disease burden and wasting medical resources. Here, we describe the pattern and dynamics of long-term complications in the lower risk subgroup of patients from the French LEA cohort of childhood acute leukemia survivors.
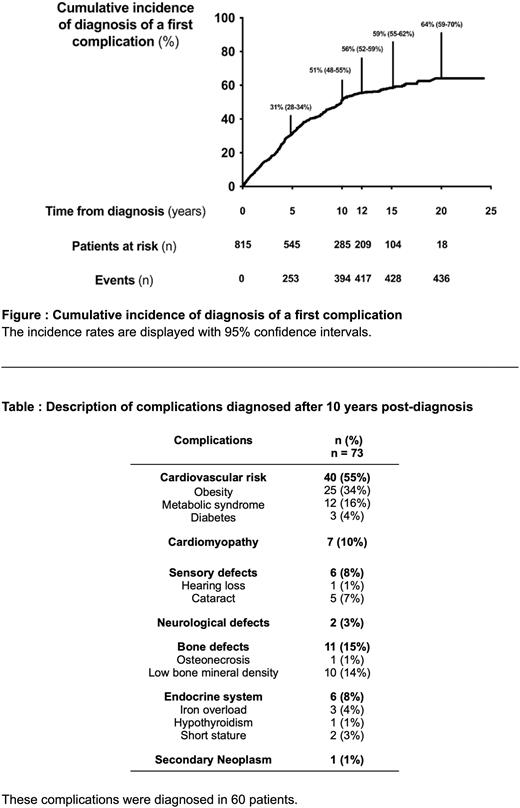
Method: LEA is a long-term follow-up program involving all childhood acute leukemia survivors treated in the French participating centers since 1980 (clinicaltrials.gov identifier: NCT01756599). The patients included in the present study were all patients included in the LEA cohort without relapsed disease and treated without CNS irradiation or HSCT, with a ≥10 years follow-up post-diagnosis and with ≥1 evaluation(s) after 18 years of age. Eighteen complications were prospectively screened during dedicated follow-up visits: cardiovascular risk factors or complications (obesity, metabolic syndrome, diabetes, coronary artery disease, stroke), cardiomyopathy, sensory defects (cataract, hearing loss), neurological defects, bone defects (osteonecrosis, decreased bone mineral density), endocrine complications (hypothyroidism, short stature, delayed puberty), iron overload, pulmonary function abnormalities, neurological complications, and secondary cancers. The cumulative incidence of long-term complications was estimated using the Kaplan-Meier method.
Results: The study included 815 patients (364 female and 451 male patients). The patients were acute lymphoblastic (88%) or myeloblastic (12%) leukemia survivors. Median age at diagnosis was 11.4 (interquartile range (IQR) 6.7-14.5) years. First and last evaluations were performed 5.1 (IQR 3.9-7.6) and 10.6 (IQR 7.9-14.5) years post-diagnosis, respectively. During follow-up, 63% of patients had ≥3 evaluations. During follow-up, 47%, 37%, 12%, 3% and 1% of patients were diagnosed with 0, 1, 2, 3 and ≥4 complication(s), respectively. Regarding usefulness of evaluations, at least one novel complication was detected in 51%, 15%, 6.3%, 5,8% and 0.0% of evaluations occurring 0-5, 5-10, 10-15, 15-20 and ≥20 years post-diagnosis, respectively (p<10-6). The cumulative incidence of the diagnosis of a first complication is shown in the Figure. At 5, 10, 15 and 20 years post-diagnosis, the cumulative incidence of diagnosis of a first complication was 31%, 51%, 59% and 64%, respectively. The cumulative incidence of diagnosis of a complication after 10 years post-diagnosis was not statistically different in the group who experienced ≥1 complication(s) before 10 years post-diagnosis versus the group who did not. Seventy-three complications were diagnosed after 10 years post-diagnosis and are described in the Table. After 10 years post-diagnosis, the most frequent and severe complications were cardiovascular risk factors (obesity (n=25/73, 34%), metabolic syndrome (n=12/73, 16%) and diabetes (n=3/73, 4%)) and cardiomyopathy (n=7/73, 10%).
Conclusion: The results of our study confirm the need for a prolonged follow-up of survivors of childhood acute leukemia even for patients at lower risk of long-term complications. The first 10 years post-diagnosis is the period of greatest risk for complications. The usefulness of follow-up visits for diagnosing long-term complications dramatically decreased over time. After 10 years post-diagnosis, cardiovascular risk factors and cardiotoxicity are the most frequent and severe long-term complications that were diagnosed. The follow-up program of lower risk childhood leukemia survivors should focus on cardiac and cardiovascular risk after 10 years post-diagnosis, particularly in resource-constrained settings. Genetic factors are probably needed to further stratify the risk of long-term complications and individualize the follow-up.
Disclosures
Dalle:Teva: Current equity holder in private company; Sanofi: Honoraria; Vertex: Honoraria; Novartis: Honoraria; Jazz Pharmaceuticals: Honoraria; Medac: Honoraria; Orchard: Honoraria. Baruchel:Novartis: Honoraria, Membership on an entity's Board of Directors or advisory committees; Kite Gilead: Honoraria, Membership on an entity's Board of Directors or advisory committees; Servier: Honoraria, Membership on an entity's Board of Directors or advisory committees; Jazz: Honoraria, Membership on an entity's Board of Directors or advisory committees; Sanofi: Honoraria, Membership on an entity's Board of Directors or advisory committees; Clinigen: Honoraria, Membership on an entity's Board of Directors or advisory committees.
Author notes
Asterisk with author names denotes non-ASH members.

This feature is available to Subscribers Only
Sign In or Create an Account Close Modal